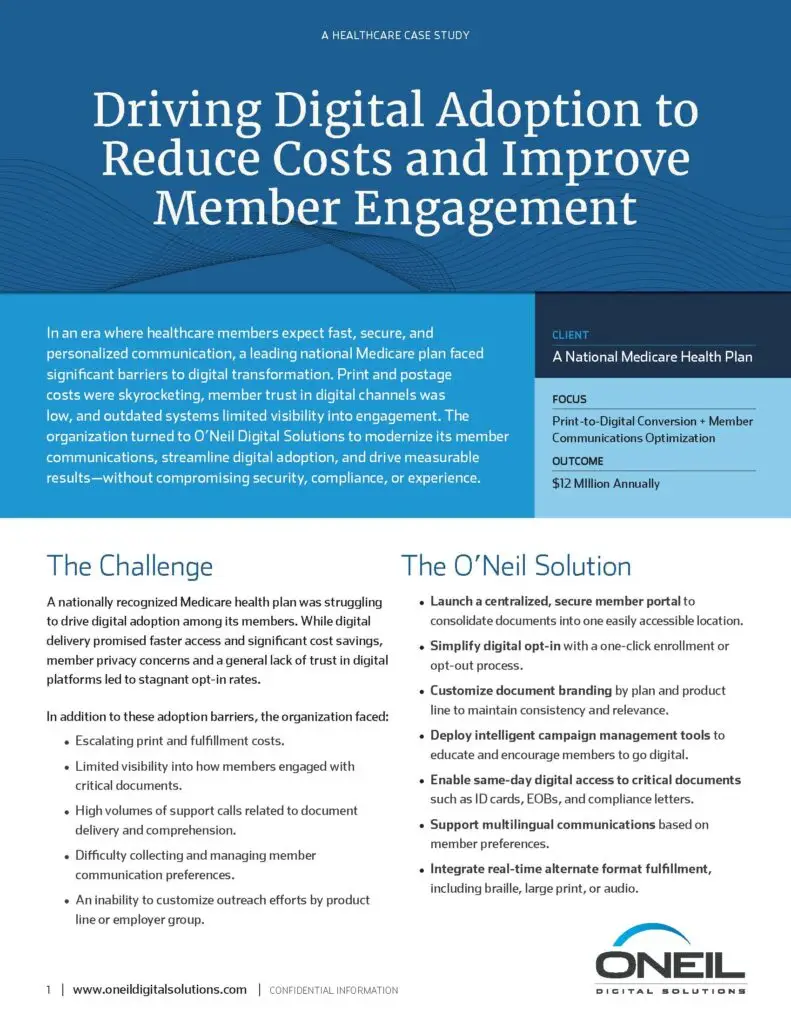
In an era where healthcare members expect fast, secure, and personalized communication, a leading national Medicare plan faced significant barriers to digital transformation. Print and postage costs were skyrocketing, member trust in digital channels was low, and outdated systems limited visibility into engagement. The organization turned to O’Neil Digital Solutions to modernize its member communications, streamline digital adoption, and drive measurable results—without compromising security, compliance, or experience.
A nationally recognized Medicare health plan was struggling to drive digital adoption among its members. While digital delivery promised faster access and significant cost savings, member privacy concerns and a general lack of trust in digital platforms led to stagnant opt-in rates.
In addition to these adoption barriers, the organization faced:
A measurable shift from paper to digital—delivering millions in savings and a stronger, more satisfying member experience.
With unified templates and smart delivery preferences, the organization strengthened regulatory compliance and reinforced brand trust at every step.
A 20% increase in member digital opt-ins led to over $1 million in monthly postage savings—totaling $12 million annually.
Simplified access and faster delivery of documents—such as ID cards and EOBs—boosted member satisfaction and reduced support call volumes.
A centralized portal and personalized campaigns made digital enrollment easy, driving higher engagement and stronger communication touchpoints.
Members gained same-day digital access to critical documents, eliminating wait times and improving transparency across the board.
By partnering with O’Neil, this Medicare plan transformed its communication model—cutting costs, simplifying digital enrollment, and significantly improving the member experience. If your organization is facing similar challenges with digital adoption or escalating print costs, we’re here to help.
Let’s talk about how O’Neil can elevate your communications strategy—while delivering measurable savings and stronger member relationships.